Critical pulmonary stenosis is a cyanotic congenital heart disease in which the pulmonary obstruction is such severe that it requires the patency of PDA for the survival of the neonate. It is a condition which requires prompt suspicion, diagnosis and management within the initial days of life. We present below a case of critical pulmonary stenosis.
5 days old, female baby was referred in view of cyanosis at day 4 of life. It was a term baby, born by normal vaginal delivery, cried immediately after birth with a birth weight of 2.4 kg at an outside hospital. The antenatal period was uneventful. The baby was discharged on day 2 of life. On day 4 of life, the baby was found to have bluish discoloration of the peri-oral region and peripheries by the mother and was advised for a pediatric cardiologist’s opinion and referred to our Centre.
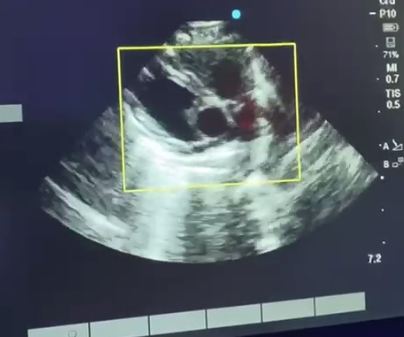
On examination, the baby did not have any dysmorphic features. Central cyanosis was evident. Vitals were stable with room air saturation of 55-60%. Echocardiographic evaluation revealed a dooming pulmonary valve with critical pulmonary stenosis with a peak gradient of 100 mm hg, post stenotic dilatation of the main pulmonary artery with a small PDA maintaining the pulmonary blood flow. Considering it to be a right-sided duct-dependent lesion, the baby was started on injection prostin to maintain the patency of the duct. This increased the saturation to 80-85% and prostin was gradually tapered and kept at a minimum.
The baby was taken for percutaneous balloon pulmonary valvuloplasty (PBPV) on day 7 of life. The procedure was done under general anesthesia with all aseptic precautions and dilatation of the valve was done by 7×20 Tyshak mini. Post dilatation the gradient decreased to 20 mm hg with trivial pulmonary regurgitation. The baby was shifted to ICU and was extubated the next day. Baby’s saturation in room air had increased to 97-99%. Feeds were established and the baby was discharged on day 10 of life. On follow up baby is maintaining saturation at room air, gaining weight without any significant gradient across the pulmonary valve.
Critical pulmonary stenosis is a serious congenital heart defect characterized by a narrowing of the pulmonary valve or pulmonary artery that obstructs blood flow from the right ventricle to the lungs. This condition is rare, with an incidence of approximately 1 in 10,000 live births, and it is more common in males than females.
Its etiology is not completely understood, but genetic factors are thought to play a role. Some cases are associated with genetic syndromes, such as Noonan syndrome or Alagille syndrome, while others are sporadic. Maternal exposure to certain drugs or infections during pregnancy may also increase the risk.
Clinical presentation of pulmonary stenosis in neonates varies depending on the severity of the obstruction. Mild cases may be asymptomatic, while severe cases may present with cyanosis, respiratory distress and poor feeding. Diagnosis is typically made by echocardiography.
The management of pulmonary stenosis in neonates depends on the severity of the obstruction. Mild cases may be managed conservatively with close monitoring, while severe cases require intervention. Balloon valvuloplasty is the most commonly used intervention for severe and critical PS. If balloon valvuloplasty did not give good results (due to dysplastic valve), the PDA stenting or BT shunt are the options.
The prognosis for neonates with PS depends on the severity of the obstruction and the presence of associated cardiac anomalies. Prompt diagnosis and appropriate management are essential in improving outcomes. Long-term management and follow-up care are also important to monitor for potential complications and ensure optimal health and development.
In conclusion, critical pulmonary stenosis is a rare but serious congenital heart defect that presents with cyanosis in neonates. Early diagnosis and appropriate management are essential in improving outcomes and minimizing potential complications.
Diagnostics
| Date | Type | Value | Unit |
|---|