My ward leaving exam for my Medicine clinical rotation during the third year of my MBBS had just got over and I was ready to leave the hospital with a skip in my step and carry on with my Saturday. Halfway through, I realized I had left my measuring tape with a friend back at the hospital, so I rushed back. His exam was still going on so I decided to wait for him outside when the examiner called me and asked me to check the pulse of the patient my friend had been assigned.
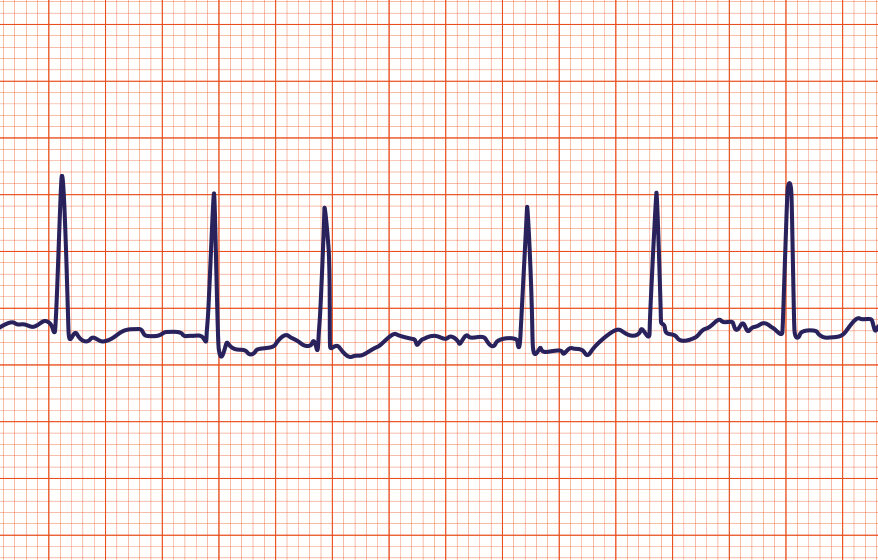
In that moment, I was a bit grumpy about being tested again after my exam had ended. Nevertheless, I went on to check the pulse and the first thing I noticed was that it was irregular. I immediately reported that and the examiner affirmed my findings and informed me that the patient was going into atrial fibrillation. In that moment, all I had learnt about ECG and tachycardias buzzed in my mind.
This was a case of a 75-year-old woman, Mrs. Santosh (name changed), whose history and examination I had done just a day before during my postings. She was a homemaker and a resident of Delhi. She had presented to the OPD with chief complaints of difficulty in breathing since 10 months and chest pain since 5 months. She was a chronic smoker and had a history of hypertension, hyperlipidemia, and chronic obstructive pulmonary disease (COPD).
PRESENTATION OF THE CASE
She was apparently normal 1 year back when she started developing breathlessness on exertion. Earlier there was slight limitation of activity, such as breathlessness on climbing stairs (NYHA Class II) which had now progressed to a marked limitation of physical activity, that is breathlessness even on walking i.e. NYHA Class III. It was associated with palpitations.
There was no history of worsening of breathlessness on lying down, and associated wheezing. There was no seasonal variation. There was no history of fever, cough or hemoptysis.
She had also been experiencing chest pain on exertion since the last six months which was central, gradual in onset, described as tightness in the chest, and non-radiating.
There was no history of syncope, cyanosis, or oedema. She was on medication for hypertension and hyperlipidemia since the last 5 years, but her son reported that she wasn’t compliant and frequently miss her doses. There was no history of diabetes mellitus or asthma.
Diagnostics
| Date | Type | Value | Unit |
|---|