Patient Presentation
A 58-year-old man presented to a local hospital in March 2022 with nausea and vomiting. Blood tests revealed:
-
Elevated white blood cell count (WBC): 25.3 × 10â¹/L
-
Low hemoglobin (HB): 65 g/L
-
High platelet count (PLT): 190 × 10â¹/L
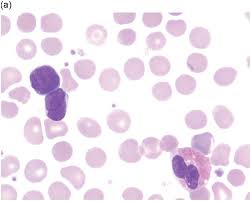
Considering these findings, doctors suspected acute leukemia. Bone marrow examination showed active mononuclear system hyperplasia with abnormal cells (51% immature mononuclear cells). Further tests identified mutations in genes associated with AML: DNMT3A, FLT3-TKD, and IDH2. A chest CT scan identified two pulmonary tuberculosis lesions.
Laboratory Findings
-
Blood counts:
-
WBC: Initially elevated (25.3 × 10â¹/L), reached a peak of 99 × 10â¹/L during treatment, then decreased to 4.1 × 10â¹/L after therapy.
-
Neutrophils: Followed a similar trend as WBC.
-
HB: Initially low (65 g/L), improved slightly to 64 g/L after anti-leukemia therapy, then significantly increased to 121 g/L after bone marrow transplant.
-
PLT: Initially high (190 × 10â¹/L), fluctuated during treatment, but ultimately increased to 242 × 10â¹/L after transplant.
-
-
Bone marrow examination:
-
Initial examination showed active mononuclear system hyperplasia with 51% abnormal cells.
-
After one course of VA regimen therapy, bone marrow tests showed improvement with only 4% primitive mononuclear cells.
-
Flow cytometry of bone marrow showed no blasts with abnormal immunophenotypes after HVA regimen therapy cycles.
-
Subsequent bone marrow tests remained normal.
-
-
Chest CT scan:
-
Revealed two pulmonary tuberculosis lesions initially.
-
Follow-up scans showed progressive reduction in lung TB foci after anti-TB therapy.
-
-
Sputum smear:
-
Initially positive for acid-fast bacillus (AFB) 3+.
-
Became negative after anti-TB treatment.
-
-
Next-generation sequencing (NGS):
-
Detected mutations in DNMT3A (48.02%), FLT3-TKD (36.3%), and IDH2 (45.95%) genes initially.
-
Subsequent tests showed varying mutation rates for these genes, but no mutations were detected in IDH2 and FLT3-TKD after HVA therapy.
-
Treatment
-
The patient received supportive care for his symptoms.
-
Due to high WBC count, he was given hydroxycarbamide to reduce it.
-
Anti-TB therapy with HRZE regimen (isoniazid, rifampicin, pyrazinamide, ethambutol) was initiated.
-
After TB was under control, the patient received anti-leukemia therapy with VA regimen (venetoclax, azacytidine). Due to drug interaction, the anti-TB regimen was adjusted.
-
The patient then underwent three cycles of HVA regimen anti-leukemia therapy (homoharringtonine, venetoclax, azacytidine).
-
Intrathecal chemotherapy with cytarabine, methotrexate, and dexamethasone was administered to prevent central nervous system leukemia.
-
Ultimately, the patient underwent a bone marrow transplant.
Outcome
Following treatment, the patient's bone marrow tests became normal, lung TB lesions showed significant reduction, and blood counts improved considerably. He then underwent a bone marrow transplant.
Diagnostics
| Date | Type | Value | Unit |
|---|